
Minimally invasive surgery

Minimally invasive surgery is a surgical method using techniques which represent the most minor possible intervention in the human body. The advantage of this surgical method is in its shortened healing period and reduced hospital stays. Minimally invasive surgery therefore provides especially patient-friendly and low-cost interventions which, however, require significantly increased complexity in terms of equipment. In many medical specialities, it has become the standard method and has replaced conventional, open surgery.
Using a device similar to an endoscope, lighting, monitoring and video transmission equipment as well as manipulation instruments such as scalpels, slings and air/fluid suction and flushing devices are introduced into the body and positioned at the surgical site through a small cut (which is why the method is also referred to as keyhole surgery). The surgical process is usually monitored and executed via three-dimensional imaging at the computer or magnetic resonance tomograph screen. Traditional endoscopic observation of the surgery via a direct visual channel is also common.
The visual specifications provide the tasks for lighting engineers: Luminance in the surgeon’s field of vision during direct visual observation through the surgical endoscope is significantly reduced due to dim lighting within the body. The same applies for video transmission from the surgical site within the body to the monitor. In both cases, the room lighting levels must be significantly reduced during minimally invasive surgery while surgical initiation requires lighting conditions appropriate for regular surgery.
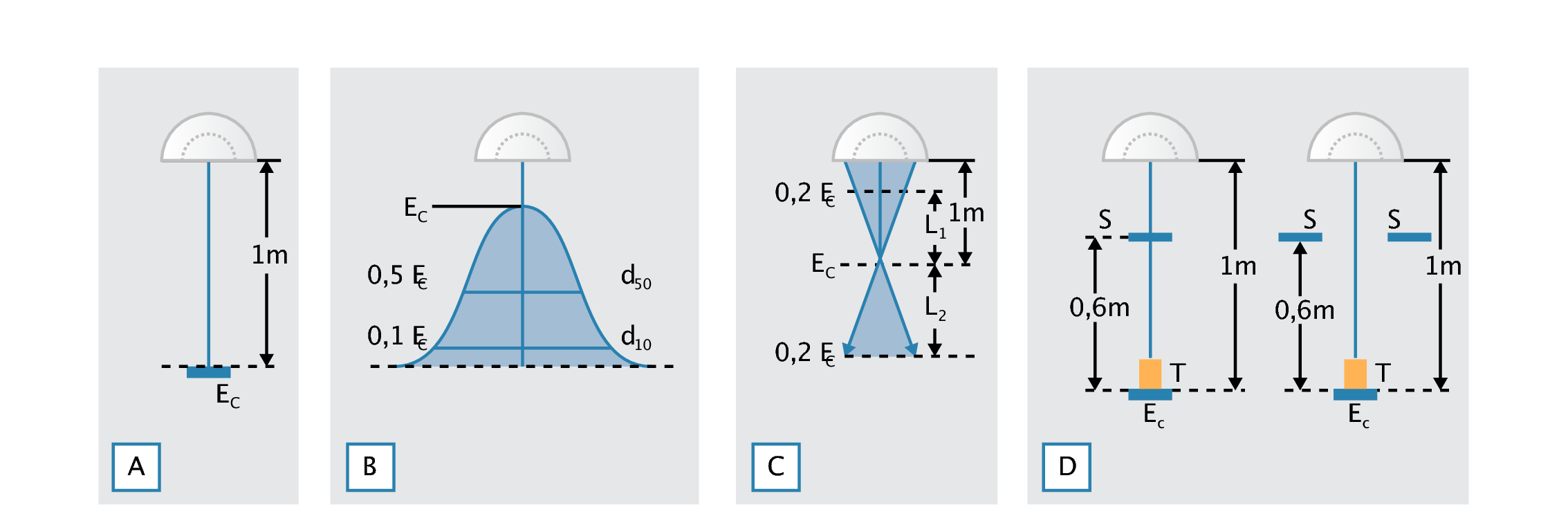
Figure 3.128: Photometric parameters for surgical luminaires according to EN 60601-2-41:
(a) Central illuminance Ec at 1 m distance from the luminaire should be between 40 klx and 160 klx.
(b) Illuminance gradient in the surgical field: At 50% of central illuminance Ec, the light field diameter d50 should be more than half the size of the light field diameter d10, where 10% of the central illuminance are achieved: d50 ≥ 0,5 · d10
(c) The light cone and its beam path. The depth of illumination L1 + L2 describes the area within the optical axis of the surgical luminaire where only 60% of the central illuminance are achieved.
(d) Shadowing effects: Using one or two matt black shadow devices S (diameter 210 mm) simulating the surgeons’ heads and one matt black cylinder T (height 75 mm, diameter 50 mm) simulating the cavity, residual illuminance in the optical axis at a distance of 1,0 m from the luminaire is determined and documented.


Figure 3.129: Multi-purpose lighting in the OR
Figure shows an operating theatre for normal and minimally invasive surgery. The high illuminance of up to 2.000 lx in the operating periphery as well as general room lighting at 1.000 lx are achieved by the cleanroom luminaires in the ceiling. A supply unit which is suspended from the ceiling provides the surgical station with all required electrotechnical installations and patient monitoring as well as gas and respiration equipment.
The supply unit features integrated general lighting, which can be regulated down to illuminance levels as low as 5 lx at the surgeons’ request. As studies at a large hospital have shown, surgeons request illuminance levels between 3 lx and 12 lx for minimally invasive surgeries. The anaesthetist’s workstation, however, requires significantly increased illuminance. It is often shielded from the actual surgical site, e.g. using drapes, so that the areas with varying lighting levels do not adversely influence each other.
For a lighting arrangement as depicted in figure, the following values were determined:
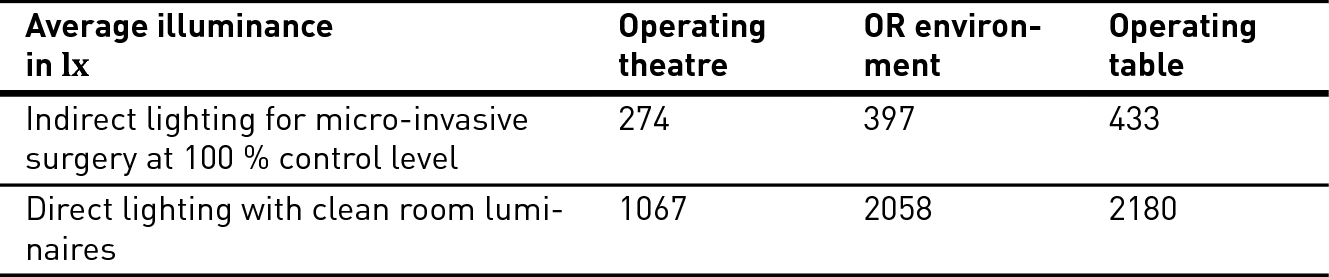
Table 3.92: Illuminance values in an operating theatre with cleanroom luminaires for direct general lighting and indirect lighting for minimally invasive surgery
In some large hospitals, green lighting is used preferentially for minimally invasive surgery. The reason: in green light, there is the least amount of disturbance in viewing the many monitors. Therefore, the globally renowned Hubertus hospital in Berlin, which specialises in minimally invasive surgery, has equipped all operating theatres in question with green light in addition to normal lighting. At the start of the actual minimally invasive surgery, the normal lighting with high illuminance is switched off. Other hospitals offering minimally invasive surgery have followed this recommendation. The green light is generated by special tubular fluorescent lamps integrated into the light fixtures for general lighting and can be switched and dimmed separately as desired.
In the multi-functional OR (figure), the distance between ceiling and supply unit is closed off with glass panels to prevent disturbances in the laminar air flow, e.g. by cross flow. This ventilation system is characterised by a high ventilation number and physiologically uncritical air speeds in the occupancy zone. It achieves maximum room air purity levels. Any obstacle within this laminar air flow (which is also referred to as piston-principle ventilation, since the air is pushed through the room from top to bottom similar to a pneumatic piston) can cause air turbulence and thus impair the efficacy of the ventilation system. This is why, instead of large-surface surgical luminaires, several small satellite luminaires are used for actual operating field lighting, which are also aerodynamically optimised.
Lighting-related recommendations for operating theatres used in minimally invasive surgery correspondingly also apply to microscope-assisted surgeries, e.g. in neurosurgery or ophthalmology.